Understanding Gynecomastia Symptoms: Diagnosis and Treatments
What are the common symptoms of gynecomastia?
Common symptoms of gynecomastia include breast swelling and tenderness, nipple discharge, and breast enlargement. It is important to note that gynecomastia may occur on one or both sides of the chest and can affect males of all ages, from infants to older adults.
What is Gynecomastia and How to Diagnose it
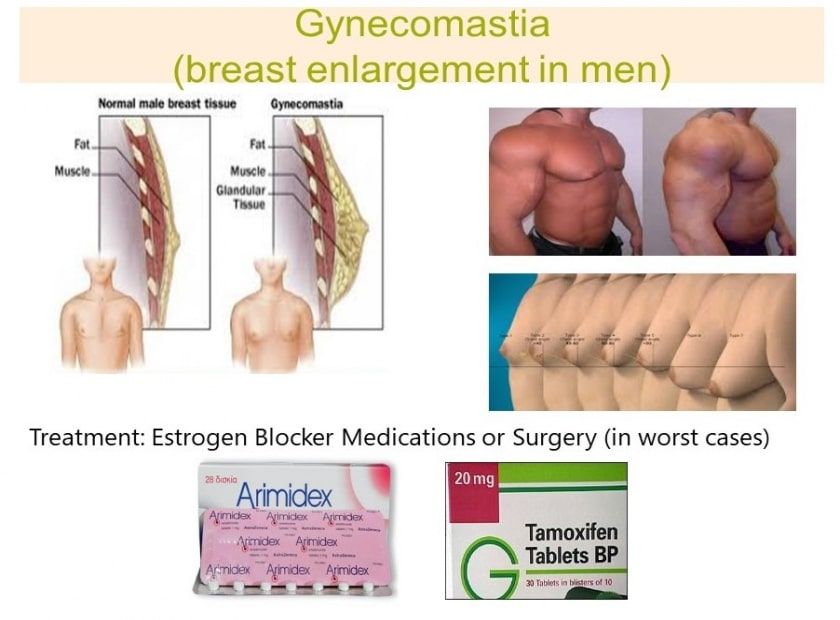
Gynecomastia is a benign enlargement of the male breast resulting from a growth of the glandular tissue of the breast, known as male breast tissue. It is defined clinically by the presence of a rubbery or firm mass extending concentrically from the nipples. At least 30% of males, including older men, will be affected during their life. Since it causes anxiety, psychosocial discomfort, and fear of breast cancer, early diagnostic evaluation of male breast tissue enlargement is important, and patients usually seek medical attention.
Evaluation of gynecomastia must include a detailed medical history, clinical examination, specific blood tests, imaging, and tissue sampling. Individual treatment requirements can range from simple reassurance to medical treatment or even surgery.
Men who start experiencing this problem complain of pain and tenderness around the nipple area. Gynecomastia was reported to cause an imbalance between estrogen and androgen action or an increased estrogen to androgen ratio, due to increased estrogen production, decreased androgen production or both, which can lead to a decrease in the level of testosterone compared with the level of estrogen. As men get older, they produce less testosterone. Older men also tend to have more body fat, and this can cause more oestrogen to be produced. These changes in hormone levels can lead to excess breast tissue growth. Androgens include testosterone and DHT. High estradiol in the presence of low testosterone and DHT, growth hormone (IGF-1 is a metabolite), and a genetic predisposition to gynecomastia can increase the size of breast tissue in men. Additionally, the lowered testosterone can cause the breast glands to enlarge and the weight gain means fatty tissue accumulates under the breast, leaving the man with a larger quantity of glandular tissue and more fat in the breast. As fat cells are estrogenic, this additional fat can further disrupt the balance between testosterone and estrogen.
Gynecomastia Causes
Physiological gynecomastia, also known as physiologic gynecomastia, is common in pubertal boys and appears to be associated with increased hormone levels of insulin-like growth factor-1 (IGF-1) and pubertal growth, but not with a shift in the balance between estrogen and testosterone, a new study suggests. Study authors noted that IGF-1 together with estrogen is essential for the growth of breast tissue, and it appears that the effect of growth hormone on breast growth is mediated through IGF-1. "The stimulatory effect of IGF-1 on breast formation was synergized by estradiol, which was also elevated in boys with physiologic gynecomastia in our study. However, serum testosterone was similarly elevated, leaving the estradiol/testosterone ratio unaltered." Prolactin, another anterior pituitary hormone integral to breast development, is not only secreted by the pituitary gland but may also be produced by normal mammary tissue epithelial cells and breast tumors (14, 15).
Testosterone converts into estradiol, DHT, and other metabolites. Men with higher amounts of the enzyme aromatase usually have this problem even at lower doses of testosterone. The growth of this glandular tissue is also influenced by a higher fat percentage, older age, excessive alcohol intake, and the use of certain medications. Gynecomastia rarely occurs in men using testosterone replacement since testosterone to estradiol ratios are improved. Estrogen levels that are too high or are out of balance with testosterone levels can cause liver disease and gynecomastia.
In several studies on testosterone replacement, only a very small percentage of people receiving testosterone experience growth of breast tissue. In one HIV-specific study conducted by Dr. Judith Rabkin in New York, she reported that out of 150 men enrolled in the study, two men experienced this adverse reaction.
Dihydrotestosterone (DHT) is a natural metabolite of testosterone that has antiestrogen activity and cannot be converted into estradiol at the tissue level. Systemic or locally administered DHT has been successfully prescribed for the treatment of patients with idiopathic and estrogen-induced gynecomastia.
Gynecomastia is also seen in men with androgen resistance with low testosterone production and DHT, where unfettered estrogen can stimulate subsequent breast development. However, in men with normal androgen receptor activity, estradiol is unable to stimulate breast development. This is thought to be due to an imbalance between the inhibitory and stimulatory effect of these hormones. Gynecomastia may be caused by abnormal hormone changes, any condition that leads to an increase in the ratio of estrogens/androgens such as liver disease, kidney failure, thyroid disease, and some non-breast tumors. Certain health conditions, like hypogonadism, can either cause or be linked with gynecomastia.
Click: Buy gynecomastia blood test panel
Gynecomastia Symptoms
Gynecomastia is a condition that causes the breast tissue in males to swell and become larger than usual. The primary symptom of gynecomastia is noticeable breast enlargement in men, which can be unilateral or bilateral. Other symptoms include tenderness or pain around the nipple area, swelling or lumps in the breast tissue, and changes in breast shape or texture. In some cases, one of the gynecomastia symptoms may also be the discharge from the nipples. If you experience any of these symptoms, it's essential to consult with a doctor to determine the underlying cause and explore treatment options.
Medications and Products That Can Cause Gynecomastia
Some medications have been reported in the medical literature to cause gynecomastia due to decreases in testosterone, increases in estradiol, or both. These include:
- · Antiandrogens.
- · HIV medications.
- · Anti-anxiety medications.
- · Tricyclic antidepressants.
- · Glucocorticoid steroids.
- · Antibiotics.
- · Ulcer medication such as cimetidine .
- · Cancer treatment (chemotherapy).
- · Heart medications such as digitalis and calcium channel blockers.
- · Anabolic steroids
- · Soy and flaxseed
- · Exposure to pesticides and byproducts of plastic processing has also been linked to increased estrogen and decreased sperm count in men.
If the cases of gynecomastia are drug-induced, gynecomastia symptoms like decreased tenderness and softening of the glandular tissue will usually be apparent within one month after discontinuation of the drug. However, if the cases of gynecomastia have been present for more than one year, it is unlikely to regress substantially, either spontaneously or with medical therapy, because of the presence of fibrosis. In such circumstances, surgical subcutaneous mastectomy, ultrasound-assisted liposuction, and suction-assisted lipectomy, including gynecomastia surgery options like liposuction, are the best options for cosmetic improvement, as described in several case series. If symptoms persist after two years or past 17 years of age, further evaluation is indicated.
During the rapid, proliferative phase, manifested clinically as breast pain and tenderness, medical therapy may be attempted. Most studies of drugs -- including testosterone (in patients without hypogonadism), have been uncontrolled and thus difficult to interpret because gynecomastia may resolve spontaneously. The few randomized, double-blind, placebo-controlled trials generally have been limited by small samples and do not disclose the potential side effects.
Gynecomastia Treatments:
Although not approved for the treatment of gynecomastia, the selective estrogen-receptor modulator tamoxifen, administered orally at a dose of 20 mg daily for up to 3 months, has been shown to be effective in randomized and nonrandomized trials, resulting in partial regression of gynecomastia symptoms in approximately 80% of patients and complete regression in about 60%. Patients in whom tamoxifen is effective usually experience a decrease in pain and tenderness within one month. In a retrospective analysis of a series of patients with idiopathic gynecomastia, 78% of patients treated with tamoxifen had complete resolution of gynecomastia, as compared with only 40% of patients receiving danazol. In case series describing the use of tamoxifen for this condition in more than 225 patients, adverse events were uncommon but can include body aches, low sex drive, and fatigue. In a double-blind study of 282 men randomized to receive 20 mg of tamoxifen once per day with bicalutamide or bicalutamide alone found that after six months, gynecomastia and breast pain were significantly reduced in men who received tamoxifen (88 versus 96 percent in the control group).
The aromatase inhibitor anastrozole was not shown to be more effective than placebo in a randomized, double-blind, placebo-controlled trial in boys with pubertal gynecomastia. Although in an uncontrolled study of 10 patients with pubertal gynecomastia, the selective estrogen-receptor modulator raloxifene was shown to result in more than a 50% decrease in the size of the gynecomastia in the majority of the boys, there are insufficient data to recommend its use at this time.
Lowering the testosterone dose had not proven helpful for the two patients in Dr. Rabkin's study. The use of antiestrogens, such as tamoxifen 10 mg twice daily, with lower doses of testosterone have been effective. Some physicians prescribe low dose aromatase inhibitors for men with early-onset gynecomastia. Gynecomastia can become permanent if the condition lasts very long although it may reduce in size when the androgen use is discontinued. In rare cases, surgical correction may be necessary in severe cases.
For men who experience enlarged breast size, doctors usually check estradiol levels to determine whether too much testosterone is being converted into estrogen. However, physicians usually forget that other hormone metabolites like DHT and IGF-1 may be involved in the development of gynecomastia, so they do not include these tests in the diagnostics panel. In order to properly diagnose gynecomastia, your healthcare provider will take your past health and medicine history and give you a physical exam. A blood test may also be recommended to check hormone levels. In some cases, a biopsy may be performed to examine the breast tissue for cancer cells, especially if there are any breast abnormalities detected during a mammogram.
Warning: Bringing estrogen down to very low levels could cause health problems in men in the long run. Hair/skin quality and health, brain function, bone density, lipids, sexual function, and other important factors may be greatly influenced by estrogen.
More information about estradiol and gynecomastia.
Bibliography:
- Braunstein, G. D., M.D. (2007). Gynecomastia. The New England Journal of Medicine, 357(12), 1229-123712
- Schulster M, Bernie AM, Ramasamy R. The role of estradiol in male reproductive function. Asian J Androl 2016;18:435-4034





