Key Pituitary And Thyroid Hormone Tests Before Starting Testosterone
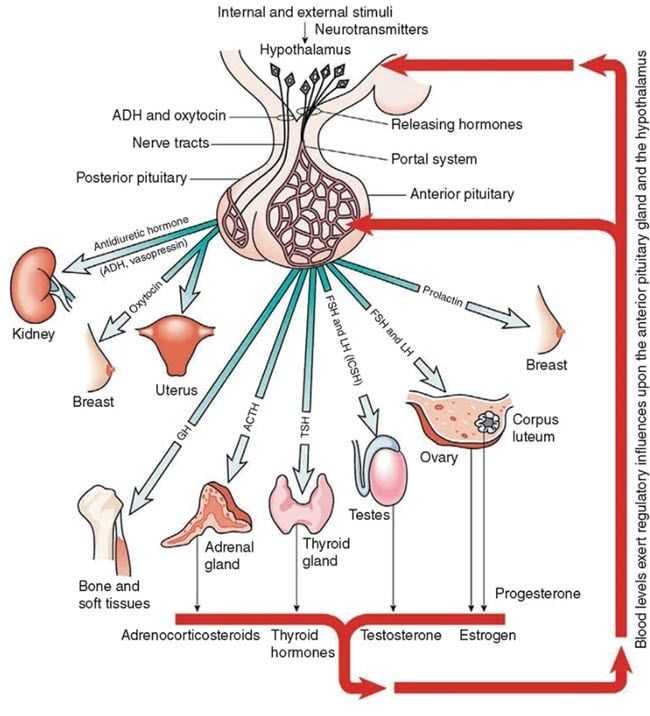
Table of Contents
- Symptoms Of Hypogonadism (Low Testosterone) And How To Diagnose
- Primary and secondary hypogonadism (Low Testosterone)
- The pituitary gland and problems associated with it
- Exploring Hyperprolactinemia (High Prolactin) and Its Implications in Low Testosterone
- Throwing a spotlight on the pituitary and its function
- Pituitary imaging in the diagnosis of low testosterone
- Learning about thyroid and its role in low testosterone
- Conclusions
Testosterone replacement therapy is available in many forms and can be beneficial for men who have low testosterone levels. When the body doesn't produce enough testosterone (a condition also known as hypogonadism), men can experience different symptoms such as low sex drive, fatigue, bad mood, and irritability.
The body might not produce enough testosterone because of different factors. For example, the pituitary and thyroid glands play an important role in the production of testosterone and if they are not healthy, young men might experience low testosterone levels.
It is important to note here that the production of testosterone decreases as men age and this is normal to be so. However, approximately 0.1% of men aged 40-49 years and about 3-5% of men aged 60-79 develop androgen deficiency which can negatively influence their lifestyle. Those who have type 2 diabetes and are obese are at a higher risk of having low blood testosterone.
Before taking advantage of testosterone replacement therapy, it is important to assess the health of other organs in the body which are directly related to the production of testosterone such as the pituitary and thyroid.
The pituitary gland is a very small organ situated at the base of the skull, weighing just 0.018 oz. It is responsible for releasing the growth hormone as well with the production of testosterone. If a patient is suspected of having low testosterone levels, doctors usually recommend analyzing and treating the pituitary gland as well, before opting for testosterone replacement (TRT) therapy.
Similarly, the thyroid is an endocrine gland situated in the neck. It is responsible for the production of numerous hormones which help the body's metabolic processes. It also plays a vital role in the production of testosterone.
Symptoms Of Hypogonadism (Low Testosterone) And How To Diagnose
This type of medical condition can have various symptoms and as mentioned earlier, people who are obese or have type 2 diabetes are more likely to develop hypogonadism. Other risk factors include chronic depression, cancer, a medicine which interferes with testosterone production, chronic illness, and others.
People who abuse opiates and glucocorticoids are also at a higher risk of developing hypogonadism over time. Proper testosterone production is strictly correlated with a healthy lifestyle, which involves working out regularly and eating a balanced diet. Smoking and cardiovascular diseases can also put someone at risk of developing low blood testosterone.
By improving the testosterone level through replacement therapy or by treating any existing pituitary or thyroid issue, the overall quality of life can be drastically increased. For example, men who have tried testosterone replacement therapy report better sexual satisfaction, better mood, more energy and a general sense of wellbeing.
In very rare cases, the testosterone level can be low because of other factors, such as extremely hard physical training. Professional athletes, especially those who compete in combat sports, might have low testosterone levels as a result of fatigue, improper nutrition, lack of rest, etc. it is important to take a look at a patient’s physical condition and training regime to accurately diagnose androgen deficiency.
A professional can use special tests to diagnose hypogonadism. It is important to let an experienced healthcare provider assess the testosterone levels to avoid confusion and medical complications.
Proper laboratory diagnosis is done early in the morning when testosterone levels are at their peak. Testosterone production follows something called a diurnal rhythm, meaning that the production is higher in the morning and lower at the end of the day. Working night shifts or having poor quality sleep can drastically influence the result of the analysis, so patients should take this into consideration. Similarly, having an acute illness can also render false testosterone diagnosis.
It is necessary to perform 2 or more testosterone evaluations to determine if a patient is suffering from hypogonadism or not, since approximately 33% of men have a positive result after one measurement.
Evaluating testosterone levels is highly recommended for certain patients, regardless if they experience the hypogonadism symptoms or not. For example, patients with HIV or those who have type 2 diabetes mellitus, osteoporosis or chronic pulmonary disease are also at a higher risk of having low serum testosterone.
Once the testosterone levels have been measured and it has been confirmed that the patient might benefit from testosterone replacement therapy, additional endocrinology tests should be performed to determine the nature of the hypogonadism – primary or secondary. Treating hypogonadism accurately is paramount, especially if the patient has certain fertility goals.
Primary and secondary hypogonadism (Low Testosterone)
As mentioned earlier, a low testosterone level in the bloodstream might result from 2 factors. The Leydig cells located in the testes are responsible for producing the majority of testosterone in men. This process takes place using the luteinizing hormone (LH) from the pituitary gland. The LH is also strictly linked to the GnRH which is produced by the hypothalamus. The GnRH is released in a pulsatile manner and a disruption in this process can lead to low testosterone levels over time.
To sum it up, men can suffer from primary hypogonadism (the testosterone is not produced in the testes), from secondary hypogonadism (the production of LH or GnRH is disrupted in the pituitary or hypothalamus) or both.
If a patient has primary hypogonadism, the LH and FSH levels will be elevated as these hormones are produced by the pituitary and hypothalamus but not properly converted into testosterone. Most specialists recommend karyotype analysis for further investigation.
The causes of primary hypogonadism can be multiple and they include HIV, toxins gathered in the body, acquired anorchia, orchitis, and more. On the other hand, if the LH and FSH levels are low, then additional investigations must be done to determine the nature of the secondary hypogonadism. It basically means that the testes are perfectly capable of making testosterone, but they don’t have the primary resource (LH) to do so.
The pituitary gland and problems associated with it
Secondary hypogonadism is a more complicated medical issue and it involves looking at the characteristics of the pituitary gland. There are numerous factors which might cause secondary hypogonadism such as certain types of tumors, untreated sleep apnea, infiltrative diseases, use of certain drugs such as marijuana, opiates, and heroin, etc.
Hyperprolactinemia can be a contributing factor in about 5% of secondary hypogonadism. This means that a prolactin adenoma can put pressure on the pituitary gland and cause damage. There are also different types of medications which can affect prolactin secretion, such as metoclopramide and others.
In some cases, secondary hypogonadism can be caused by GnRH deficiency which happens as a result of damage to the hypothalamus. This part of the brain can become injured as a result of toxins accumulation, trauma, taking certain types of medication, as well as systemic disease. If a patient is suspected of having secondary hypogonadism, he will receive a full pituitary workup to determine prolactin levels and to see if its secretion is disrupted or not.
It is paramount to differentiate between secondary hypogonadism originating in the pituitary and the one originating in the hypothalamus. Men who have fertility goals and want to have children in the near future need a different type of treatment than those who don’t have any fertility goals.
There are rare instances when men suffer from a combination of primary and secondary hypogonadism. This might happen as a result of alcohol abuse, sickle cell disease, and more. There are several treatment options available in this case such as spermatogenesis and others.
Exploring Hyperprolactinemia (High Prolactin) and Its Implications in Low Testosterone
It has been discovered that men who suffer from hyperprolactinemia experience a wide variety of symptoms, such as decreased sperm mobility and low libido. These can lead to a low-quality sex life and fertility problems. Even in the presence of relatively normal testosterone levels, hyperprolactinemia can have a significant negative impact on sexual health, leading to erectile dysfunction in worst cases.
By normalizing prolactin levels, scientists have discovered that testosterone levels improve and the overall quality of life is enhanced as well. Correct prolactin levels are directly associated with a healthy testosterone metabolism. Therefore, patients who have low serum testosterone should seek treatment for improving prolactin levels first before opting for testosterone replacement therapy. Once it has been discovered that the body responds well to hyperprolactinemia treatment, it might not be necessary to take advantage of testosterone replacement therapy.
Throwing a spotlight on the pituitary and its function
The pituitary gland plays a vital role in the production of testosterone and it should be properly assessed to determine if there are any additional hormonal imbalances present in the body. For example, for men with a testosterone level lower than 150 ng/dL, an evaluation of the anterior pituitary axes is highly recommended. This evaluation can discover other medical conditions, such as hypopituitarism, which might affect proper testosterone production.
Testing the pituitary gland should be done early in the morning before 9 am. This is done by drawing blood to measure cortisol levels as well as ACTH. If the patient works night shifts, which might compromise the accuracy of the test, an ACTH stimulant is administered intramuscularly.
This test can give insights into the hormonal balance of the patient. For example, if it is suspected that the patient has Cushing syndrome, the doctor might recommend a 1 mg dexamethasone suppression test. If acromegaly is suspected (growth hormone deficiency), then other tests are necessary to determine the exact levels of growth hormone.
Such tests are required to determine the full biochemical makeup of the patient in relation to the pituitary gland and hypogonadism. If the results are positive for one or more of those tests, the patient will be redirected to endocrinology for additional measurements.
Pituitary imaging in the diagnosis of low testosterone
Magnetic resonance imaging (MRI) might be used to discover further details about the pituitary gland and this decision is based on multiple tests of the hormone levels. Pituitary imaging is done only when proper clinical management is required and it can be used to discover incidentalomas, which can be 6 mm in diameter or less. These are small bodies that might grow on the pituitary gland and put pressure on it which in turn disrupts the regular flow of hormones required for healthy testosterone production.
These incidentalomas are usually found in approximately 20% of autopsies and can also be encountered in up to 10% of the population who is referred to pituitary imaging. The MRI testing of the pituitary should be done on men who have severe secondary hypogonadism (testosterone levels are below 150 ng/dL, persistent hyperprolactinemia, and others). Pituitary imaging isn’t necessary for cases of primary hypogonadism and it is only performed when absolutely necessary.
Learning about thyroid and its role in low testosterone
The thyroid is very important when it comes to testosterone production. In general terms, hypothyroidism has been associated with a decrease in total testosterone levels, while hyperthyroidism might lead to converting too much testosterone into estradiol, which results in impaired sexual function, gynecomastia (enlarged man’s breasts), and other medical conditions.
In some cases, hypothyroidism can lead to hyperprolactinemia, but such occurrences are rare. When this happens, improving the thyroid function through certain treatments or medication can stabilize prolactin levels and this, in turn, will normalize testosterone production.
Hypothyroidism is also frequently associated with erectile dysfunction. Similarly, hyperthyroidism can also be problematic, as it has been associated with ejaculatory dysfunction, as shown in a study done on over 750 men. More than 50 percent of those who had hyperthyroidism also showed symptoms of reduced sperm mobility and ejaculatory problems. However, when these men received treatment for hyperthyroidism, their fertility and testosterone production improved significantly, which means that testosterone replacement therapy isn't necessarily the go-to treatment for all men suffering from androgen deficiency.
Conclusions
As presented in this article, the human body is very complex, and there might be multiple causes for a low serum testosterone level in the bloodstream on males of all ages. It is important to determine whether the hypogonadism is primary or secondary, as well as perform numerous tests and hormone evaluations to determine the nature of the hypogonadism and to prescribe the correct treatment.
In case the pituitary gland is the culprit, MRI tests might be required, though such instances are rare. Certain types of treatments are also recommended if the patient has fertility goals. If none of the other medications and treatments for hypogonadism are accurate, then testosterone replacement therapy might be considered for certain patients.
By the way, monitoring serum testosterone, LH, FSH and prolactin is very easy these days thanks to tests that can be bought online at discounted prices. Visit www.discountedlabs.com for more details.





